What Is DPG Rubber Allergy and How Can You Avoid It?

Diphenylguanidine (DPG) is a rubber accelerator linked to allergic contact dermatitis. Learn how to identify symptoms, avoid triggers, and manage reactions effectively.
Contact allergies are an increasing concern, particularly in occupational settings where repeated exposure to chemical compounds can lead to adverse skin reactions. One such compound gaining attention recently is 1,3-diphenylguanidine (DPG).
1,3-Diphenylguanidine (DPG) is a chemical used to manufacture synthetic rubber to improve its strength and flexibility. While helpful in product durability, DPG is increasingly linked to allergic skin reactions, especially in people who frequently handle rubber-containing items like gloves, footwear, or face masks. Recognizing and managing this allergy is essential for individuals and employers in at-risk industries.
What Is DPG and Where Is It Found?
DPG is a rubber accelerator used in the vulcanization process, which strengthens rubber by heating it with sulfur. DPG is often combined with other chemicals like thiurams and carbamates to speed up this process.
Everyday products containing DPG include:
-
- Medical gloves (especially nitrile and neoprene)
- Rubber footwear and insoles
- Elastic in clothing and masks
- Household items (rubber bands, hoses, cords)
- Industrial tools with rubber parts
Because DPG is usually not listed on labels, people may unknowingly come into contact with it. Even brief skin contact with DPG-treated materials can trigger a reaction in individuals with sensitivities, making awareness and proactive avoidance key to prevention.

Skin Reactions from DPG
DPG can cause allergic contact dermatitis, a delayed skin reaction. Symptoms typically appear 1 to 3 days after exposure and may include:
-
- Erythema and pruritus (redness and itching)
- Swelling or papules or vesicles (small fluid-filled blisters)
- Cracking or Lichenification (thickened, leathery skin) with ongoing exposure
Common exposure areas include:
-
- Hands and wrists (from gloves)
- Feet (from shoes or insoles)
- Face and neck (from masks or elastic bands)
These reactions may be mistaken for other skin issues, like eczema or irritation from friction or sweat. However, specific patterns—such as where the rash appears and how long it lasts—can offer important clues, especially when there’s regular contact with rubber gloves, footwear, or equipment.
Diagnosing DPG Allergy
Patch testing is the most accurate way to confirm a DPG allergy. This involves applying small amounts of suspected allergens, including 1,3-diphenylguanidine, to the skin (usually the back) under occlusion for 48 hours, followed by readings at 48 and 72–96 hours to assess for delayed hypersensitivity reactions.
Testing can also identify sensitivities to related rubber chemicals such as:
-
- Thiurams
- Carbamates
- Benzothiazoles
Because individuals may be sensitized to multiple rubber additives, testing for a broader spectrum when rubber allergy is suspected, particularly in occupational cases, is crucial.
Several conditions can mimic the appearance of DPG-induced allergic contact dermatitis, making differential diagnosis essential. These include:
-
- Irritant contact dermatitis (from sweat, friction, or harsh soaps)
- Atopic dermatitis (especially in those with a history of eczema)
- Fungal infections (especially on the feet)
Distinguishing these conditions requires a careful clinical history, consideration of the patient’s occupational and environmental exposures, and confirmation through patch testing. Early and accurate diagnosis can significantly reduce symptom recurrence and improve quality of life by guiding allergen avoidance.

Who Is at Risk?
Occupational exposure is a significant risk factor. High-risk groups include:
-
- Healthcare workers: Frequent use of rubber-based gloves (especially nitrile or neoprene) puts nurses, doctors, and lab technicians at high risk.
- Industrial laborers: People in automotive, manufacturing, or construction industries may encounter DPG through rubber parts, conveyor belts, hoses, or protective gear.
- Food service and janitorial staff: These roles often involve prolonged glove use, especially during cleaning, dishwashing, or food preparation.
- Footwear and textile workers: Employees making or handling rubberized shoes, insoles, or elasticated textiles may develop sensitization through dermal contact.
- Hairdressers and beauticians: Using rubber gloves during chemical treatments can expose these workers to DPG and related accelerators.
Even outside of work, DPG can show up in everyday items. Some things to watch for include:
-
- Rubber-lined shoes or insoles that may cause foot irritation
- Elastic in waistbands, socks, or underwear
- Personal gear like face masks, goggles, or sports headbands
- Household items with rubbery textures, such as remote controls, yoga mats, or kitchen tools
Being aware of these sources helps reduce the risk of unexpected flare-ups.
Managing DPG Allergy
Two things matter most when treating DPG contact allergy: easing the current symptoms and avoiding future contact with the allergen. Since the reaction usually appears a day or more after exposure, the best approach is to stop contact early and manage flare-ups with topical treatments, as a healthcare provider advises. Long-term, avoiding DPG products is the most effective way to stay symptom-free.
Short-Term Relief:
-
- Topical corticosteroids or calcineurin inhibitors for inflammation
- Moisturizers and barrier creams to repair the skin
- Oral antihistamines to reduce itching
- In severe cases, short-term oral steroids
Long-Term Strategies:
-
- Use accelerator-free gloves (vinyl or special nitrile)
- Choose clothing and shoes without rubber or elastic components
- Request material safety data sheets (MSDS) to identify DPG in products
- Use cotton liners under gloves or socks as a barrier
Patient education is a vital part of long-term care. Dermatologists and allergists should help patients identify likely sources of DPG exposure in their daily routines and recommend suitable alternatives to reduce skin contact with sensitizing materials.

Choosing Safer Alternatives
People with DPG allergies don’t have to give up convenience—just make smarter swaps. Look for:
Accelerator-Free Gloves and Medical Supplies
In clinical and occupational settings, many manufacturers offer accelerator-free gloves, specifically designed for users with sensitivities. These gloves are often made from:
-
- Vinyl: A synthetic material that skips the vulcanization process, so it doesn’t need rubber accelerators at all.
- Accelerator-free nitrile: Specially manufactured nitrile gloves that omit all standard accelerators like DPG, thiurams, carbamates, and benzothiazoles.
- Polyethylene: Used in short-duration tasks, although less durable than nitrile or latex.
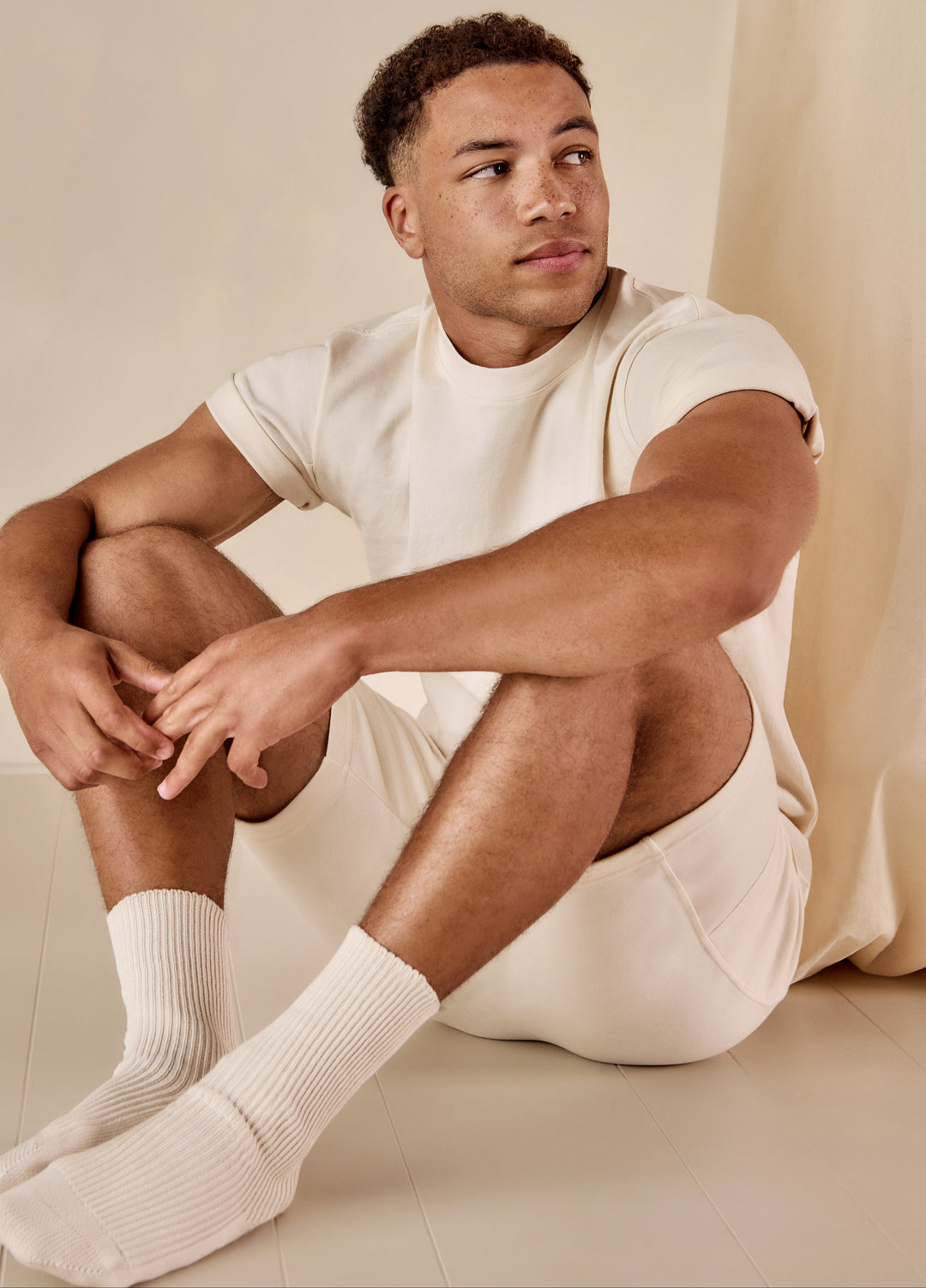
Textile and Footwear Options
Clothing and footwear choices can also play a significant role in minimizing skin exposure. Recommendations include:
-
- Latex-free and elastic-free garments: Choosing clothing made entirely from non-elastic textiles, such as 100% organic cotton, helps reduce contact with hidden accelerators.
- Non-rubber footwear and insoles: Leather, canvas, cork, or textile-based options without rubber soles or padding can be safer for those with foot dermatitis.
- Socks and undergarments without elastic bands: Some specialty brands offer garments specifically designed for individuals with textile and chemical sensitivities.
Everyday Products to Watch Out For
DPG can show up at home in more places than you might expect. Some everyday items to be mindful of include:
-
- Yoga mats, resistance bands, and tool handles with rubber grips
- Headbands, straps, or mask ear loops that contain stretchy rubber
- Electrical cords or kitchen tools with soft, rubber-like coatings
Some brands also label their gloves as “dermatologist-tested” or “hypoallergenic,” but users should verify claims and check for accelerator-free labeling or certifications where possible. These changes can make a real difference in avoiding flare-ups.
DPG allergy often flies under the radar, but it’s something many people deal with, sometimes without knowing the cause. Recognizing familiar sources and choosing better alternatives can go a long way in managing symptoms. People can regain control and live more comfortably with more explicit product labeling, accurate diagnosis, and greater awareness.
DISCLAIMER: The information provided on Cottonique’s website is intended solely for general informational purposes and should never be considered a substitute for professional medical advice, diagnosis, or treatment. All content—including text, treatments, outcomes, charts, graphics, photographs, and study findings—is created for educational purposes and should not be regarded as establishing a standard of care.
Readers are encouraged to verify any information from this site with reliable sources and consult their physician or a qualified healthcare professional regarding any medical condition or treatment. As part of its mission to help individuals with allergies live more comfortably, Cottonique emphasizes the importance of seeking personalized medical advice for any health concerns.